Health Sciences North is located in the Ramsey Lake Health Centre in Sudbury. Photo: Health Sciences North/Facebook
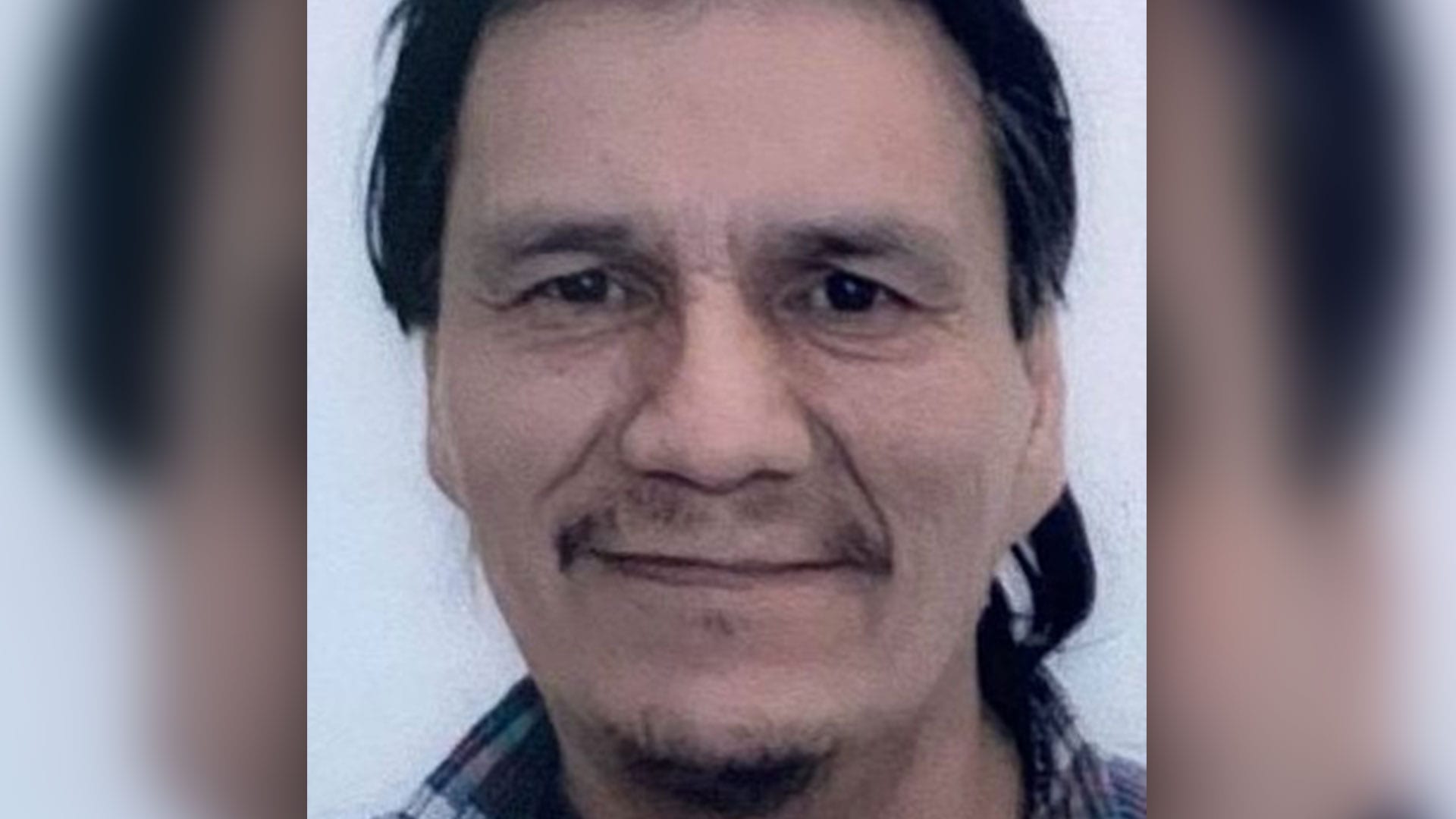
Accessing health care in Attawapiskat may not always be easy but for Dominic Hookimaw it became a nightmare.
Hookimaw, 54, needed urgent medical care after he was the victim of an assault that left him with head, neck, back and leg injuries in late March.
A medevac to Sudbury, Ont., turned into a weeks-long ordeal of frustration, confusion and fear for the resident of the remote Cree community along the James Bay coast.
“I was not feeling well when I was discharged,” said Hookimaw from his home in Attawapiskat, where he’s slowly on the mend. He spoke in Cree while his sister Jackie Hookimaw-Witt interpreted.
He was released two days after admission, given a bottle of antibiotics and told to head home.
“I was achy, I had a fever and I didn’t really know what was going on,” he added. “I didn’t understand what the pills were for that were provided to me. It was just confusing.”
But Hookimaw proved unfit to travel. His condition worsened. He wound up in the Sudbury hospital again and, eventually, sought care in North Bay that he felt was superior.
It left Hookimaw and his family upset, seeking answers and out of pocket thousands of Indian Day School settlement dollars.
“I don’t want somebody to go through what I went through. It was horrible,” said Hookimaw. “I ask all the people that work for the health services, whether it’s Aboriginal medical care, whether it’s FNIHB or the hospital, to please listen when we ask for help.”
APTN News reviewed medical records alongside an account of the events and allegations written by Hookimaw-Witt, his sister.
APTN also reached out to Health Sciences North in Sudbury, which provided a detailed response below.
First admission to Sudbury ICU
Hookimaw, who speaks little English, was admitted to the ICU on March 29 where he was diagnosed with a head injury. He was also diagnosed with alcoholism and tobacco addiction, according to patient discharge papers.
He was released from the ICU two days later. The discharge document said he “improved significantly overnight and apart from a small headache, he is able to independently ambulate and does indeed want to go home.”
The plan was for him to stay at a local Travelodge hotel before catching a bus to Timmins then flying back to Attawapiskat. He was prescribed an antibiotic and sent on his way.
Hookimaw had a mild fever of 39 C, his sister said, which made travel complicated due to the pandemic. Hookimaw-Witt said her brother and their other sister weren’t provided with the discharge papers, which were obtained later, and weren’t sure what the pills were for.
Hookimaw-Witt argued that her brother ought to have been monitored with more rigour because he was diagnosed with a “closed head injury secondary to assault,” according to the discharge papers.
“He couldn’t travel anyway because he was sick,” said Hookimaw-Witt. “They told us if you don’t go on the bus (to Timmins), you’re on your own. And I said, ‘Well OK. I have to look after my brother.’ But I made sure to keep all the documents.”
Hookimaw did not travel home. The brother and sister dipped into their Indian Day School Settlement cash to pay for food, travel and lodgings. Hookimaw-Witt estimated she spent over $2,000 out of pocket.
“Imagine if the person was on welfare or elderly and they have no money. What do they do?” she said over the phone. “My brother went from ICU to the street in Sudbury. And that’s unacceptable.”
At the Travelodge his condition deteriorated rapidly. He experienced weakened legs and back pain, said Hookimaw-Witt.
On April 5, he wound up back in Sudbury hospital after a referral from a walk-in clinic. There he was prescribed naproxen (an anti-inflammatory) for the pain but no mobility device to help walk.
Hookimaw-Witt also believes he ought to have been put on a liquid diet to the swelling in his throat.
Second opinion in North Bay
Soon after that, the siblings travelled to North Bay to stay with relatives and save money while Hookimaw recovered.
Here they sought a second opinion and received what they felt was superior care.
“We felt really looked after (in North Bay) and that they were acknowledging our Nativeness, our name, our language. It felt great,” said Hookimaw-Witt. “The doctor was great too. She answered all the questions, and she saw that we were scared what those antibiotics were for.”
Dominic agreed in Cree as relayed by his sister.
“I didn’t feel well looked after until we went to North Bay. Things changed,” he said. “It got better there.”
In North Bay they were able to access the discharge papers and received a more thorough explanation, said Hookimaw-Witt.
In emails sent to APTN, she said a doctor in North Bay took Hookimaw off the naproxen anti-inflammatory. He was prescribed a muscle relaxant for the legs and back instead.

Then a different doctor at the North Bay emergency room advised them not to travel, referred them for physiological and neurological assessments, and prescribed Hookimaw with crutches and a walker before returning home, said his sister.
He had his final assessment in North Bay on April 22 and then finally went home the next day — nearly a month after originally scheduled — she said in her written account.
The ordeal left them feeling neglected and dissatisfied with the standard of care.
“You can tell he’s Aboriginal and he doesn’t speak much English. And because he couldn’t talk, he was stuttering,” she said of her brother when he was first admitted. “All this would contribute to stereotyping. He couldn’t talk because he had a swollen neck and it was irritated.”
In her written account of events, she warned them that the outcome could have been serious had she not been there to help.
“Other patients do not have the luxury of having somebody in the family who, due to her education, is able to find the facts,” Hookimaw-Witt wrote.
“He had no clue what was actually going on in his body and thus he would have been prevented to do a follow-up.”
Sudbury Health Sciences North responds
After reviewing all this, APTN emailed the Sudbury hospital and laid out the family’s concerns.
The hospital responded that they can’t comment on specifics of any one patient’s care due to provincial privacy legislation.
“What we are able to say is that HSN (Health Sciences North) is dedicated to providing a culturally safe environment that supports diversity and inclusivity for patients, visitors and staff,” said the hospital in a written statement.
“As such we take complaints related to discrimination very seriously and would encourage anyone who has felt they have not received proper care or been mistreated to follow up directly with our Patient Relations Department.”
The statement went on to say that the hospital is committed to engaging with Indigenous communities and has a strategic plan to improve Indigenous health outcomes. It said the hospital hired a director of Indigenous heath last winter, renovated a new medicine lodge and has Indigenous liaisons who can help patients navigate the system.
“Through these positions, we also have access to a Cree interpreter for patients who would prefer to receive services in this language,” said the statement. “HSN continues to work to honour and strengthen our partnerships and relationships with the Indigenous communities we serve.”
After Hookimaw-Witt relayed the comments to her brother, he replied in Cree that this was news to him.
“I don’t believe it because, from my experience when I was in the ward at ICU, there was no Cree person,” Hookimaw said. “There was no Indigenous person that came to see me throughout the time I was there. I felt isolated. There was culture shock and a language barrier. So, I don’t really believe the statement that was released from the hospital based from my personal experience.”
Hookimaw-Witt expressed concern about the institutional inequality that exists in Canada. Both Treaty 9 and the Canadian Charter of Rights and Freedoms ought to guarantee free and universal access to medical care for all citizens, she said.
“For us, it’s different. I don’t know if it’s because of the colonial institution that we’re dealing with. The health-care system is flawed with institutional racism,” she said.
“We’re treated as wards of the state.”
APTN followed up with the hospital asking whether or not they are looking into the complaints.
We also asked them to respond to Hookimaw’s comment that he did not receive any of the cultural services mentioned in the statement, but received no response by the time the story was published.