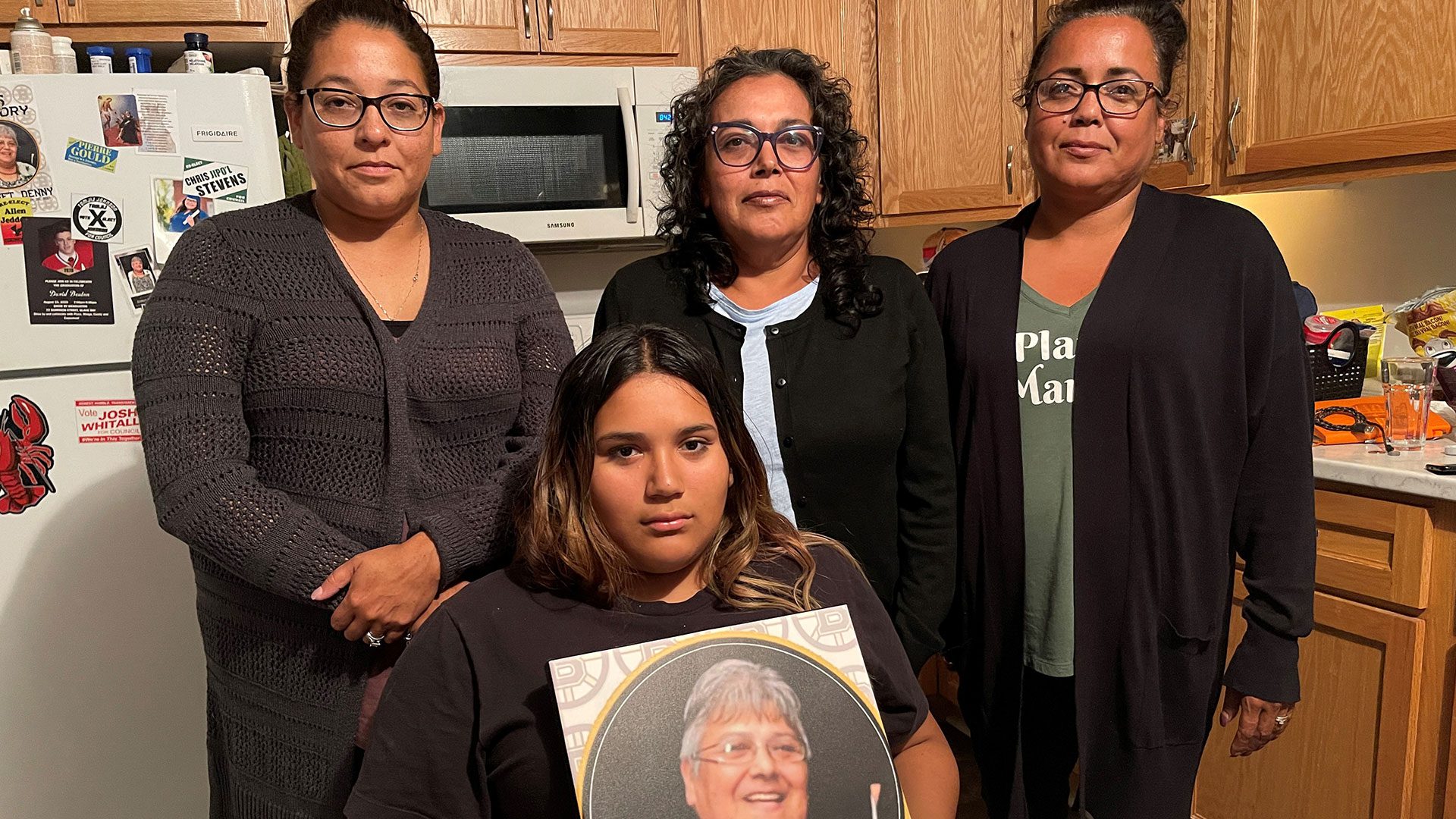
MaryI Joe-Francis says she was shocked when the provincial investigation into the death of her mother-in-law, Bridget Denny, found the hospital failed to provide adequate care.
“And I question myself all the time, what if there was a non-Native person in there, would they have you know would they have answered the buzzer, would they have run, you know you don’t know, you question this stuff because we’re First Nation people, we live with racism every day and it’s in the back of your mind you just wonder what if, what if,” said Joe-Francis.
Denny, 65, died unexpectedly while in care at the Cape Breton Regional Hospital on Jan. 20, 2021.
Denny, a residential school survivor, mother of five, grandmother to 15, Mi’kmaw language speaker, and an active member of her community, the Eskasoni First Nation, went to the Cape Breton Regional Hospital on Jan. 19, 2021, for pain and complications from her diabetes.
Her body was cremated. Days later, before the funeral, the family found out from another patient that Denny had fallen in the middle of the night.
The family obtained Denny’s medical chart, then filed a complaint with the Nova Scotia College of Physicians and Surgeons of Nova Scotia
Lynette Reid, assistant professor of bioethics at Dalhousie University, said, healthcare has a long past of discrimination.
“When people already have a history of receiving racist care from the healthcare system when they already have a history of receiving inadequate care, then that inadequate care is more harmful for them,” said Reid.
Tajikeimik, a Mi’kmaw health organization, works with the Nova Scotia government to improve healthcare.
Executive director Lindsay Peach said healthcare needs to change.
“Working with the provincial health systems around the complaints process so that there is a true picture and understanding of the extent of racism and what that looks like in the health system, how that impacts people’s care experience, how it impacts the quality and safety of the care that they receive,” said Peach.

Joe-Francis said Denny was afraid to go to the hospital,
“It makes me sad as a Mi’kmaw woman, for our elders, for my parents the fear the fear to go to a place that is supposed to care for you, that blows my mind, no elder should ever be scared to go to a hospital,” said Joe-Francis.
The incident sparked an investigation under the Protection for Persons in Care Act.
A final report issued on Feb. 25, 2021 concluded:
“The facility failed to provide adequate care based on the lack of documentation … in response to the affected patient’s unwitnessed fall, including failing to document the affected patient’s post fall vitals and post fall assessments firsthand, staff inaccurately completed the affected patient’s admission fall risk assessment and hourly checks, and no documented evidence that post fall neuro vitals and a SIMS report were completed.”
The report also said, “it is beyond the scope of this investigation to determine if this contributed to the affected patient’s death.”
According to the report, “around 2 a.m. another patient was ringing their call bell, while standing in the doorway attempting to get the attention of the staff, saying, ‘someone is on the floor here’ and ‘someone needs help in here.’”
Staff arrived and helped Denny Back to bed.
The report continued, “the person implicated documented second-hand information about the fall as “patient slid to the floor,” however, “the fall was consistently reported as being unwitnessed, therefore, investigators were unable to determine how the fall occurred and the length of time the affected patient was on the floor.”
The report said there is no documentation Denny was assessed after she fell, or staff followed the hospital’s fall and injury prevention policy, which includes:
“A head to toe assessment, monitoring for injuries especially for an un-witnessed fall … for 48 hours after fall, monitoring involves vital and neurovital sign assessments every two hours at a minimum, and documentation of details of the fall in the patient health record chart and the incident reporting system,” according to the report.
Read More:
Family wants answers after Mi’kmaw grandmother dies unexpectedly in Cape Breton Hospital
According to the report, the nursing flow chart indicated Denny was in bed and did not get up to go to the washroom between 7 p.m. and 6 a.m, which contradicts the progress note and staff reports.
Reid said paperwork matters,
“One thing didn’t happen here and then 20 things couldn’t happen afterwards, but that just shows you the importance of that one thing, paperwork is never just paperwork in the healthcare system,” said Reid.
The next morning, Denny was unresponsive and could not be revived.
The report said, “had the physicians known about the fall, the file would have been reported to the medical examiner, and the family would have chosen to proceed with an autopsy.”
Joe-Francis said the family was not informed about Denny’s fall.
“No one had ever said she fell; no one had said she had a rough night; no one ever said her blood pressure was low, nothing, there was nothing other than she was a very sick woman and that’s all we were told,” said Joe-Francis.
Joe-Francis says the family wants to hire a lawyer, but can’t find one. She said they’re too busy or in a conflict of interest.
Reid said the lack of lawyers available to families is for a reason,
“They have most of the competent health lawyers in the country on retainer, so that is a known barrier to access for accountability for patients because there are not that many lawyers that have competence in health law that are available to patients to pursue lawsuits,” said Reid.
The report included five directives for the hospital, but with no deadline.
The directives include training staff patient medical record documentation, fall and injury prevention policy, compliance with unexpected death policy, duty to report abuse, signs of abuse, and reporting procedures ti the PPCA.
The Nova Scotia Department of Seniors and Long-term Care said in an email statement to APTN News:
“The department will continue to actively monitor the situation until the directives are fully addressed.”
Joe-Francis said that is not enough.
“They couldn’t even let her die with dignity, and that is the most heartbreaking part about it because, the system is our healthcare system, they failed not only our mother-in-law, my mother-in-law, their mother, our grandmother,” said Joe-Francis.
The Denny family said it’s considering all legal options.